Today vs Tomorrow
NEUROMODULATION OVERVIEW
Neuromodulation Today
Neuromodulation therapies are used to treat various conditions, including chronic pain, Parkinson’s disease, overactive bladder, and epilepsy. While some patients experience relief, the current standard of care suffers from 3 key limitations.
LIMITATION 1
Invasive Surgery
While neuromodulation has produced positive outcomes for some patients, the burden of surgery can have serious consequences. Neuromodulation devices are placed with highly invasive surgical procedures. Procedure time ranges from 17 to 283 minutes (Bina et al. 2020, Schönburg, Bukethal, Fornana 2020), and often requires large (>1cm) incisions and sutures, imparting infection risk to the patient. Moreover, it has been shown that scarring, including surgical scars, was associated with low self-confidence, self-consciousness, anxiety, and feelings of despair (Brown et al. 2008).
Chronic conditions have been associated with high incidence of anxiety and depression (Mullins, Yong, Bhattacharyya 2020, Vrijens et al. 2015); thus, invasive surgery may further exacerbate their symptoms. After surgery, patients are advised to clean and monitor the surgical site, and minimize lifting, bending, and stretching to prevent lead migration. During this recovery period, some patients rely on loved ones and caregivers to assist with activities of daily living and aid in the recovery process by changing wound dressings (Hoffmann, D’Souza, & Hagedorn, 2022).
LIMITATION 2
Complicated Procedures
Neuromodulation leads are often manufactured with hooks or tines to grip the issue upon placement, or manually anchored with deep fascial sutures or “S'' tension loops (Chapman et al. 2021, Deer et al. 2014), requiring clinician expertise built on years of experience and dedicated training (Pritzlaff et al. 2023). In addition, these procedures are time-intensive to achieve appropriate device placement and anchoring (17-283 min). Even when clinicians are appropriately trained and regarded experts in the field, lead migration and fracture are still common occurrences. In some instances, patients undergo revision surgery to remove or replace the lead, which may require invasive surgery (Chmiela et al. 2021). Thus, clinicians and patients are in a cycle of invasive surgery restricted by complicated techniques.
LIMITATION 3
Last Resort
Many neuromodulation therapies require prior payer approval due to surgical implant cost. Reimbursement coding requires several conditions to be met, including “used only as a late resort (if not a last resort)” for spinal cord stimulators (CMS, 1995), and “documented failure of less invasive treatment modalities and medications” for peripheral nerve stimulators (CMS, 2019). Thus, patients must exhaust treatment options, including physical therapy, pharmaceutical intervention via oral drugs and injected drugs, which has been reported to take 5 years of debilitating suffering after the onset (Kumar et al. 2013). Chronic conditions have been associated with negative workplace experiences (Sebasta et al. 2022) and reduced quality of life (Mullins, Yong, Bhattacharyya 2020, Vrijens et al. 2015). While neuromodulation is a promising approach, reimbursement indications inhibit broad access to patients.
Neuromodulation Tomorrow
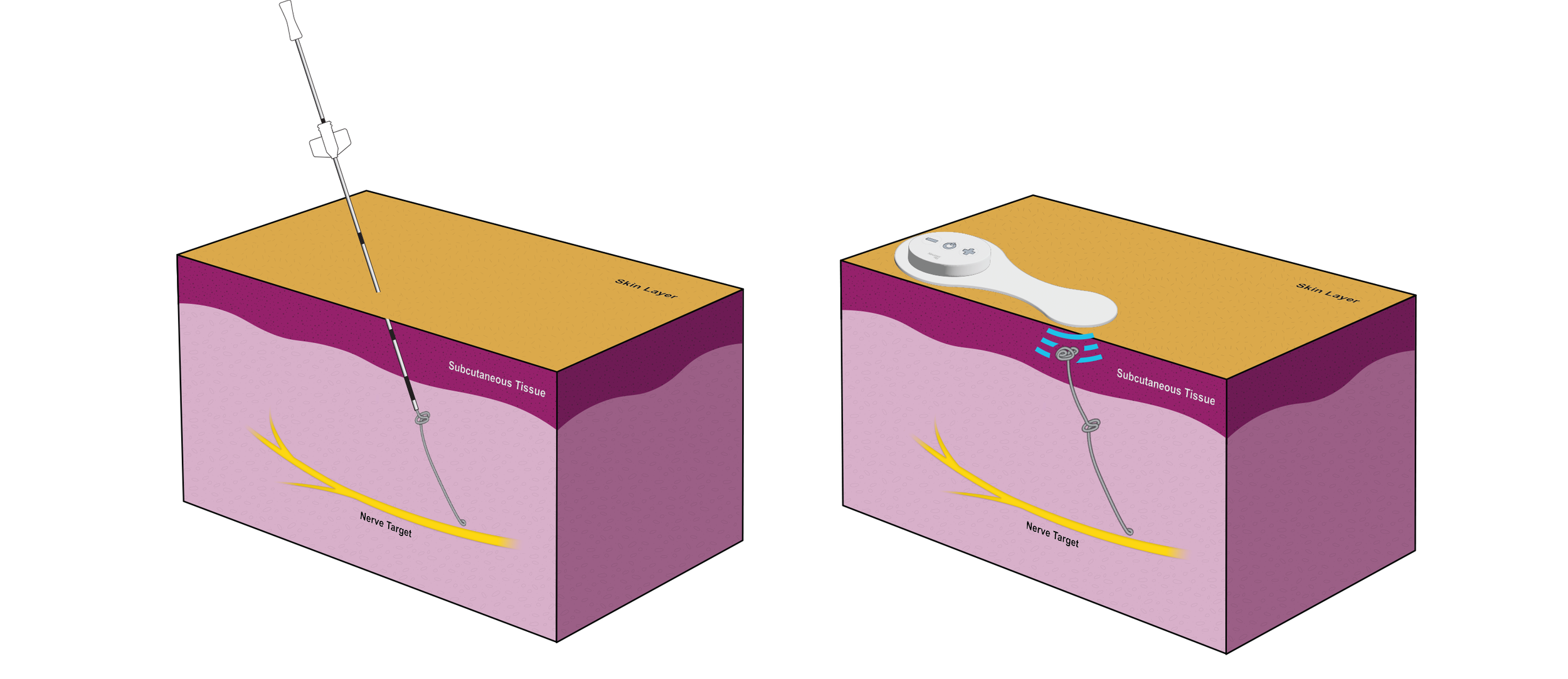
Neuromodulation will be as easy as a drug injection. Placement and removal will be done by needle, removing the need for surgery, saving time, money, and the patient from scars.
Minimally Invasive & Needle-Based
Neuromodulation devices are placed with needle-based delivery systems. The placement method does not require any large incisions (<5mm) or sutures, leaving no visible scars. Devices can be placed during an in-office visit. Patients return to their activities within 1 day of device placement, with no need to change wound dressings.
Simple Procedure
Neuromodulation devices can be placed and removed with known procedures, as simple as a steroid injection. Neuromodulation leads are self-anchoring, without hooks, tines or sutures. The incidence of lead migration and fracture are minimized, with fewer patients undergoing revision and undue burden. Clinicians can place and remove neuromodulation devices without specialized training or years of experience.
Earlier Intervention
There is a paradigm shift in which patients are eligible for neuromodulation therapy sooner in the treatment timeline due to its simplicity and minimally invasive nature. Patients may still experience negative effects of chronic conditions, but become eligible for neuromodulation sooner than 5 years after the onset of their condition. Patients need to demonstrate that they’ve pursued alternate treatment options prior to a neuromodulation device, but the barrier to entry is reduced. When repeated steroid injections don’t provide adequate relief, patients can try neuromodulation to see if they respond to therapy. If they respond, they keep the device, with the option of an implanted IPG. Otherwise, the device can be removed with a minimally invasive in-office visit.